Background: Acute lymphoblastic leukemia (ALL) is a cancer of lymphoid cells and organs that requires immunochemotherapy combined with hematopoietic stem cell transplantation (HSCT) according to minimal residual disease. Recently, cell therapy and targeted drugs have been added to the treatment algorithm. Supportive care, and local treatment such as intrathecal chemotherapy are also recommended due to complications related to disease and therapy.
Introduction: The Peripherally Inserted Central Catheters (PICC )may be a safe and useful tool for the treatment of ALL patients because it is easier to implant with a lower risk of complications than Centrally Inserted Central Catheters (CICC), and is effective in outpatient settings.
Methods: Since its introduction in our medical oncology department, a PICC team consisting of a hematology physician and three dedicated nurses has conducted a prospective study to evaluate the efficacy and complication rate of the PICC system in inpatients and outpatients ALL. Inclusion criteria included all ALL patients who required chemotherapy, supportive care, or HSCT, regardless of white blood cell (WBC) count. A platelet count (PLT) greater than 20000/mm 3 and normal coagulation tests were required for implantation. In all patients, the vascular anatomy of the arms was previously examined by ultrasound. All implantations were performed under ultrasound control, followed by radiographic control.
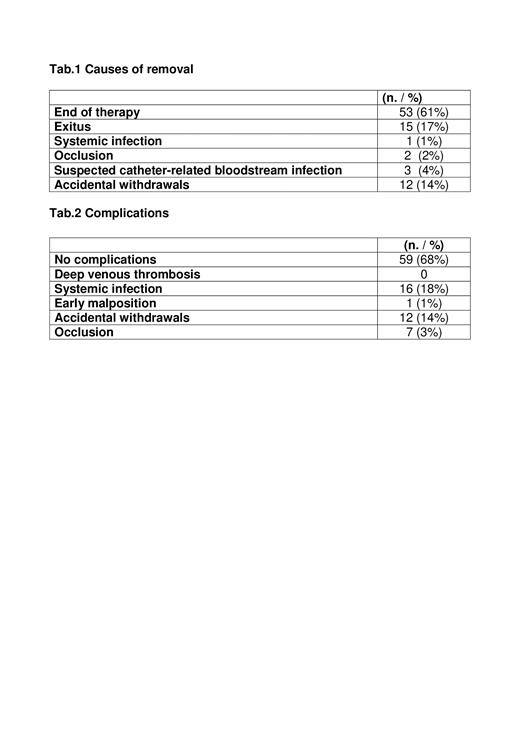
Results: From March 2007 to April 2023, 87 PICC implantations were performed in 75 patients, including 39 men and 36 women. The mean age was 44 years (range 15-80). The majority of implantations were performed in hospitalized ALL patients (81-93%). Seventy-one PICCs (82%) were used for chemotherapy, eleven (13%) for supportive care, two (2%) for autologous HSCT, 4 (5%) for allogeneic HSCT. No PICC was lost to follow-up. At the time of this analysis, only one PICC (1%) was still in situ and in use. Total PICC survival was 13683 days (median, 121; range, 1-1257). The reasons for removal are listed in Table1. Of note, most PICCs were removed because of end of therapy (61%) and exitus (17%), and only 1 in 3 (33%) had suspected catheter-related bloodstream infection confirmed by microbiological testing. Complications recorded in the overall populations are described in the Table.2
No complications occurred in 68% of PICCs. There were 16 episodes of confirmed PICC-related systemic infection recorded (18%; 1.1/1000 days/PICC). The pathogens isolated in blood cultures and in analysis of PICC spikes were: Staphylococcus Epidermidis, Staphylococcus Hominis, Pseudomonas Aeruginosa, Escherichia Coli, Enterococcus Faecium, Klebsiella Pneumoniae, Candida spp. Only 1 of 16 confirmed PICC-related systemic infections (6%) required removal of the devices, whereas in the other 15 cases (94%), PICC were allowed to remain after resolution of the infection with systemic antibiotic therapy. No cases of symptomatic thrombotic complications associated with PICC were recorded.
Conclusions: These data suggest that the use of PICC can be considered the device of choice in the treatment of ALL patients because it is easy to insert, safe to use, durable, and associated with a low complication rate, even in the case of PICC-related systemic infections.
Disclosures
No relevant conflicts of interest to declare.